What is a Clinical Trial in Cancer Care? A Complete Guide for Patients

Receiving a Cancer diagnosis often brings overwhelming emotions and countless questions about treatment options. While your oncologist will likely discuss standard treatments like surgery, chemotherapy or radiation, you may also hear about clinical trials. Understanding what clinical trials are and whether they might be right for you is an important part of making informed decisions about your Cancer care.
This comprehensive guide will help you understand clinical trials in Cancer treatment, how to find them and what to expect if you decide to participate.
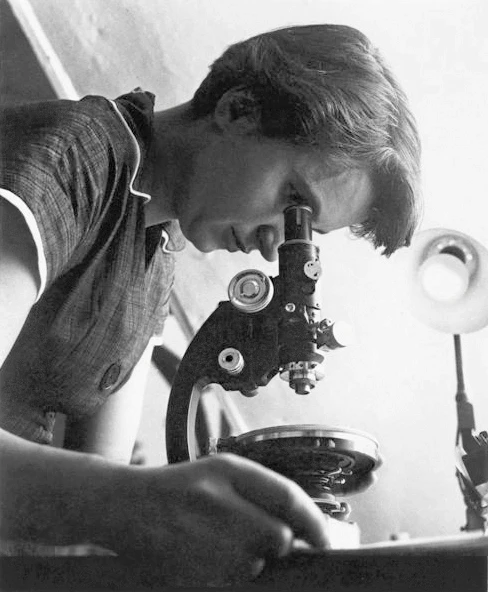
Understanding Clinical Trials: The Foundation of Medical Progress
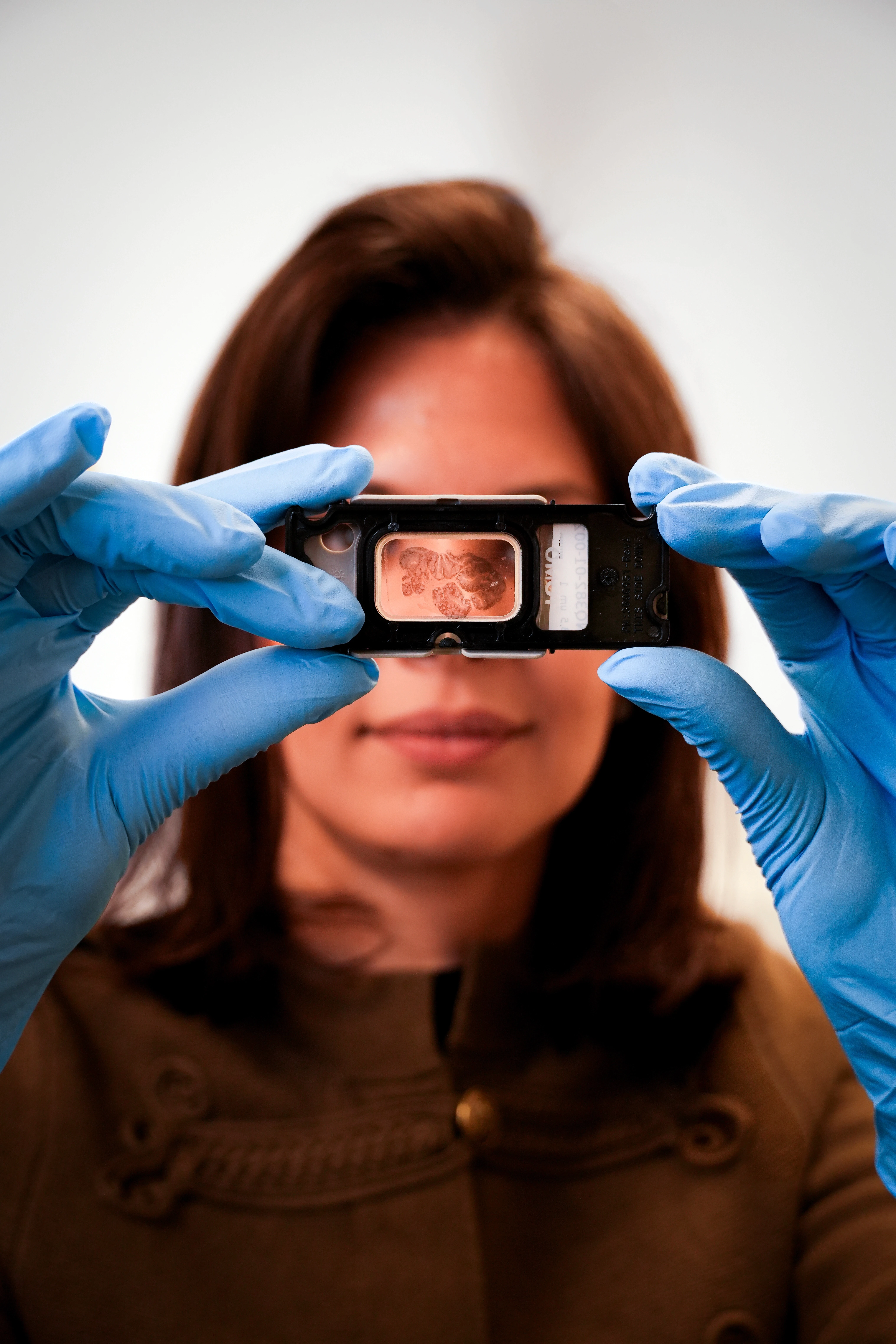
A clinical trial like our Rosalind Study is a carefully designed research study that investigates new ways to prevent, detect or treat Cancer. These studies are the cornerstone of medical advancement, testing whether new Cancer treatments are safe and effective before they become widely available to patients.
Every Cancer treatment available today, from chemotherapy drugs to targeted therapies and immunotherapies, went through the clinical trial process. When you participate in a clinical trial, you're potentially accessing cutting-edge treatment options and contributing to research that may help future Cancer patients.
Why Clinical Trials Matter in Oncology
Cancer research has made remarkable progress in recent decades, and clinical trials are the engine driving this advancement. Through these studies, researchers have developed:
Targeted therapies that attack specific Cancer cell mutations
Immunotherapy treatments that harness your immune system to fight Cancer
Less toxic chemotherapy regimens with fewer side effects
Precision medicine approaches tailored to individual tumor characteristics
Improved diagnostic tools for earlier Cancer detection
Without clinical trials, these innovations would never reach patients who need them.
Types of Cancer Clinical Trials
Not all clinical trials serve the same purpose. Understanding the different types can help you identify which studies might be relevant to your situation.
Treatment Trials
These are the most common type of Cancer clinical trial. Treatment trials test new drugs, drug combinations, surgical techniques, radiation approaches or other therapies. They aim to find treatments that are more effective, cause fewer side effects or improve quality of life compared to existing options.
Prevention Trials
Prevention trials study ways to reduce Cancer risk in people who haven't been diagnosed with Cancer but may be at higher risk. These might test medications, vaccines, lifestyle changes or dietary supplements.
Screening and Early Detection Trials
These studies evaluate new methods for detecting Cancer earlier, when it may be more treatable. They might test new imaging technologies, blood tests, or genetic screening approaches.
Diagnostic Trials
Diagnostic trials investigate better ways to identify Cancer or determine its characteristics, such as testing new biomarkers or imaging techniques that help guide treatment decisions.
Quality of Life Trials
Also called supportive care or palliative care trials, these studies focus on improving comfort and quality of life for people living with Cancer. They may test ways to manage symptoms, side effects or psychological challenges.
The Four Phases of Clinical Trials: A Step-by-Step Process
Cancer treatment trials typically progress through four distinct phases, each with specific goals. Understanding these phases can help you evaluate the potential risks and benefits of participating.
Phase I Trials: First Steps in Human Testing
Phase I trials are the first time a new treatment is tested in humans, usually involving 15-30 participants. These studies primarily focus on safety, determining:
What dose is safe to use
How the treatment should be administered
What side effects occur
How the body processes the treatment
Phase I trials often involve patients whose Cancer hasn't responded to standard treatments. While the primary goal is safety rather than effectiveness, some participants do experience benefits.
Phase II Trials: Evaluating Effectiveness
If a treatment proves safe in Phase I, it moves to Phase II trials with 25-100 participants. These studies assess:
Whether the treatment works against specific Cancer types
What response rates look like
More detailed safety information
Which patients are most likely to benefit
Phase II trials help researchers decide whether a treatment is promising enough to warrant larger studies.
Phase III Trials: Comparing to Standard Treatment
Phase III trials are large studies involving a couple hundred to thousands of participants. They compare the new treatment to the current standard of care to determine:
Whether the new treatment is more effective
How side effects compare
Whether it improves survival or quality of life
Which patient groups benefit most
Successful Phase III trials often lead to regulatory approval and widespread availability of new treatments.
Phase IV Trials: Post-Approval Monitoring
After regulatory approval, Phase IV trials continue monitoring a treatment's long-term safety and effectiveness in real-world settings with thousands of patients.
How to Find Clinical Trials: Your Path to Potential Options
Finding relevant clinical trials for your specific Cancer type and situation requires some research, but several resources make this process more manageable.
Clinical Trial Database Resources
The primary resource for finding Cancer trials is a clinical trial database. Several international databases list studies from around the world, allowing you to search by:
Cancer type and subtype
Location and country
Treatment approach
Trial phase
Eligibility criteria
Many countries and regions maintain their own clinical trial registries, and international databases aggregate studies from multiple sources worldwide. Your healthcare provider can guide you to the most relevant clinical trial database for your region. For example:
Clinical Trial Matching Services
Searching through thousands of studies can feel overwhelming, which is where clinical trial matching services become valuable. These platforms use your specific information, including Cancer type, stage, genetic markers, previous treatments and other factors, to identify trials that might be appropriate for you.
Many Cancer centers and organizations offer clinical trial matching services to help patients:
Identify relevant studies based on their unique situation
Understand clinical trial eligibility requirements
Connect with trial coordinators
Navigate the enrollment process
Clinical trial matching services use advanced technology to connect patients with appropriate opportunities based on their individual Cancer characteristics and treatment history.
Working with Your Healthcare Team
Your oncologist and Cancer care team are invaluable resources when searching for clinical trials. They can:
Recommend trials based on their knowledge of your case
Provide referrals to institutions conducting relevant research
Help you evaluate whether a trial is appropriate
Coordinate with trial investigators on your behalf
Ask your doctor about clinical trial options. If they aren't aware of relevant studies, they can often consult with colleagues or refer you to specialists who are.
Understanding Clinical Trial Eligibility: Who Can Participate?
Each clinical trial has specific clinical trial eligibility criteria that determine who can participate. These requirements ensure the study can answer its research questions while protecting participant safety.
Common Eligibility Factors
Clinical trial eligibility typically depends on:
Cancer-Related Factors:
Cancer type and subtype
Stage and extent of disease
Specific genetic mutations or biomarkers
Previous treatments received
Response to prior therapies
Health-Related Factors:
Overall health status and organ function
Other medical conditions
Current medications
Age requirements
Performance status (ability to carry out daily activities)
Logistical Factors:
Geographic location and ability to travel to the study site
Availability for required visits and tests
Insurance coverage considerations
Why Eligibility Criteria Exist
While eligibility requirements can feel restrictive, they serve important purposes:
Scientific validity: Ensuring the study can answer its research questions
Safety: Protecting participants from unnecessary risks
Comparability: Creating groups that can be meaningfully compared
Regulatory compliance: Meeting requirements for regulatory approval
Even if you don't meet criteria for one trial, you may qualify for others. Clinical trial eligibility varies significantly between studies, so it's worth exploring multiple options.
The Screening Process
Determining your eligibility involves a screening process that may include:
Medical history review
Physical examination
Laboratory tests and imaging studies
Review of pathology reports
Discussion of previous treatments
This screening ensures the trial is appropriate for you and that you're a suitable candidate for the study.
How to Enroll in Clinical Trials: The Step-by-Step Process
Once you've identified a promising trial and confirmed your potential eligibility, the process to enroll in clinical trials involves several important steps.
Initial Contact and Pre-Screening
First, you or your doctor will contact the trial coordinator listed in the study information. The coordinator will conduct an initial pre-screening, usually by phone, to review basic eligibility criteria and answer your questions about the study. It is also frequent that a trial coordinator will approach you or your doctor to enroll you in an ongoing study.
Formal Screening Evaluation
If pre-screening suggests you might be eligible, you'll undergo formal screening. This typically involves:
Visiting the trial site
Meeting with the research team
Undergoing medical tests and evaluations
Providing detailed medical history
Screening can take several days to weeks, depending on the study requirements.
Informed Consent Discussion
Before enrolling, you'll participate in an informed consent discussion with the research team. They'll explain:
The study's purpose and procedures
Potential risks and benefits
What's required of participants
Your rights as a research participant
Alternative treatment options
You'll receive a detailed informed consent document to review, and you should feel free to ask questions, take time to consider your decision, and discuss it with family members or your primary oncologist.
Enrollment and Randomization
If you decide to proceed and meet all eligibility requirements, you'll formally enroll in the study. For trials comparing treatments, you may be randomly assigned to receive either the experimental treatment or standard care. This randomization process ensures unbiased results.
Important Considerations When Enrolling
Before you enroll in clinical trials, consider:
Time commitment: Clinical trials often require more frequent visits than standard care
Travel requirements: You may need to visit the study site regularly
Insurance coverage: Understand what costs are covered by the trial versus your insurance
Impact on daily life: Consider how participation fits with work, family, and other commitments
What to Expect During a Clinical Trial
Understanding what happens during trial participation can help you feel more prepared and confident in your decision.
Treatment and Monitoring
Throughout the trial, you'll:
Receive the study treatment according to the protocol
Undergo regular monitoring visits
Complete questionnaires about symptoms and quality of life
Have laboratory tests, imaging studies and physical exams
Keep detailed records of any side effects or health changes
The Research Team's Role
Your trial research team typically includes:
Principal investigator (lead doctor overseeing the study)
Research nurses and coordinators
Data managers
Other specialists as needed
This team works closely with your regular oncology team to coordinate your care.
Your Rights as a Participant
As a clinical trial participant, you have important rights:
The right to ask questions at any time
The right to withdraw from the study for any reason
The right to privacy and confidentiality
The right to be informed of new information about the study
The right to continue receiving appropriate care if you leave the study
Weighing the Benefits and Risks
Participating in a clinical trial involves potential benefits and risks that you should carefully consider with your healthcare team.
Potential Benefits
Access to new treatments before they're widely available
Close monitoring by a specialized research team
Contribution to Cancer research that helps future patients
Some costs may be covered by the trial
No-cost access to the study treatment
Potential Risks
The new treatment may not be effective for you
Unknown or unexpected side effects may occur
More frequent visits and tests than standard care
You may receive a placebo or standard treatment rather than the experimental therapy (in randomized trials)
Insurance may not cover all trial-related costs
Common Questions and Concerns
Will I receive a placebo instead of treatment?
In Cancer clinical trials, particularly for patients with active disease, placebos are rarely used alone. When trials include a control group, participants typically receive either the standard treatment or the standard treatment plus the experimental therapy. Your informed consent document will clearly explain whether a placebo is involved.
Can I continue with my current oncologist?
Yes. Most clinical trials work in coordination with your primary oncology team. The research team manages the study treatment while your regular doctor continues overseeing your overall care.
What if the trial doesn't work for me?
If the trial treatment isn't effective or causes unacceptable side effects, you can withdraw and pursue other treatment options. Your medical team will help you transition to alternative therapies.
Are clinical trials only for people who have run out of options?
No. Clinical trials exist for all stages of Cancer and all points in the treatment journey. Some trials test treatments for newly diagnosed patients, while others focus on advanced disease. You don't need to have exhausted all standard options to participate.
How much will it cost?
The study treatment and research-specific procedures are typically provided at no cost. However, standard care costs (routine tests, doctor visits) are usually billed to your health insurance as they would be for any Cancer treatment. The financial aspects vary by country and healthcare system, so trial coordinators can help you understand what costs are covered before you enroll.
Making Your Decision: Is a Clinical Trial Right for You?
Deciding whether to participate in a clinical trial is deeply personal. Here are some questions to discuss with your healthcare team:
How does the trial treatment compare to my standard options?
What are the potential benefits specifically for my situation?
What are the risks and how do they compare to standard treatment?
How will the trial affect my daily life and responsibilities?
What happens if I experience side effects or the treatment doesn't work?
Am I comfortable with the level of uncertainty involved?
Remember, participating in a clinical trial is always voluntary. You can take time to make your decision, discuss it with loved ones, seek second opinions and ask as many questions as you need.
Moving Forward with Knowledge and Support
Clinical trials represent hope and progress in Cancer care. They offer potential access to innovative treatments while advancing research that benefits all Cancer patients. Understanding what clinical trials are, how to find them through clinical trial databases and matching services, what determines clinical trial eligibility, and how to enroll in clinical trials empowers you to make informed decisions about your Cancer care.
If you're interested in exploring clinical trial options, start by:
Discussing trials with your oncologist
Searching clinical trial databases for relevant studies
Considering clinical trial matching services to identify appropriate opportunities
Contacting trial coordinators to learn more about specific studies
Taking time to carefully evaluate whether participation aligns with your goals and values
Your journey with Cancer is unique, and your treatment decisions should reflect your individual situation, preferences and priorities. Whether you choose to participate in a clinical trial or pursue standard treatment options, what matters most is that you feel informed, supported and confident in your decisions.
Clinical trials have brought us every Cancer treatment advance we have today, and they continue to offer promise for better outcomes tomorrow. By understanding your options and working closely with your healthcare team, you can make the choices that are right for you.
To read more about our Exceptional Voices Committee
To read more about our Networks
Updated: Jan 27, 2026


